All Bills
All Bills
All Bills is the bills of all Consultation Lab Pharmacy Procedure Package Rad
Surgery Other charges is mentioned.
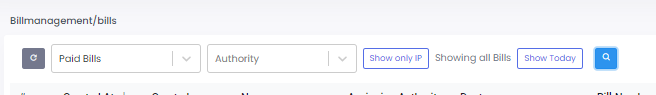
Refresh : This command updates the current view or data set to display the most recent information. It ensures that all displayed data, such as bills and payments, is up-to-date.
All Bills : This category includes every bill generated by the hospital, regardless of its current status. This can include paid, pending, refunded, and cancelled bills.
Paid Bills : These are bills that have been fully settled. Payments have been received and processed, and no outstanding amount is due.
Pending Bills : Bills that have been issued but have not yet been paid. These may be awaiting payment from patients, insurance companies, or other entities.
Refunds : This category includes any bills where payments have been
reimbursed. This could happen due to overpayment, billing errors, or
cancellations where payments were already made.
Cancelled Bills : Bills that have been voided or annulled. No payment is
required for these bills, possibly due to administrative errors or other
reasons.
Authority : This typically refers to the entity or individual responsible for the bill or the approval of transactions. In a hospital setting, it could refer to the department or personnel with the authority to approve payments, refunds, or cancellations.
Show All : A command that displays all records within the specified category. For instance, if in the context of bills, it would show all bills regardless of their status (paid, pending, refunded, cancelled).
Show Only IP (Inpatient) : This filter limits the view to only the bills related to inpatient services. Inpatients are those who are admitted to the hospital for at least one overnight stay.
Show Today : This filter displays only the bills or transactions that were created or modified on the current date.
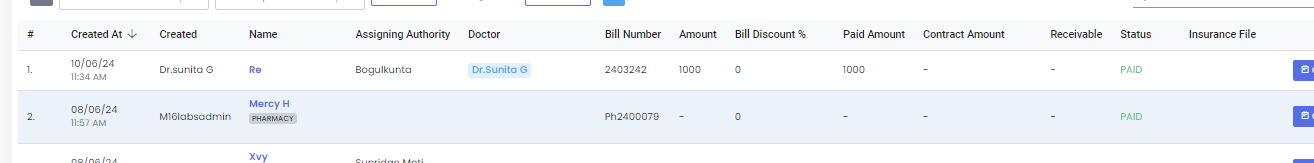
Created At : This refers to the date and time when the bill was generated. It helps in tracking the billing history and organizing records chronologically.
Created By : This denotes the person or system that generated the bill. It could be a hospital staff member, or a doctor or billing department employee.
Name : This is the name of the patient for whom the bill is issued. It helps in identifying the patient associated with the particular bill.
Assigning Authority : This is the entity or individual who authorized or assigned the bill. It could be a department head, a doctor, or an administrative authority within the hospital.
Doctor : This field indicates the name of the doctor responsible for the patient’s treatment. This is important for linking the medical services provided with the respective medical professional.
Bill Number : A unique identifier assigned to each bill. This number is crucial for tracking and referencing specific bills within the hospital’s billing system.
Amount : The total cost of medical services and treatments provided to the patient before any discounts or payments are applied. It represents the gross amount billed.
Bill Discount% : This is the percentage of discount applied to the bill. Discounts might be provided for various reasons, such as promotional offers, financial aid, or insurance agreements.
Paid Amount : The amount of money that has been paid towards the bill by the patient, their family, or through insurance. This reduces the total amount owed.
Contract Amount : This could refer to a pre-agreed amount between the hospital and the patient or their insurance provider. It often comes into play with insurance companies that have a set contract rate for specific treatments.
Receivable : The remaining amount that is still owed by the patient after accounting for any paid amounts and discounts. This represents the outstanding balance on the bill.
Status : The current status of the bill, which could be ‘paid’, ‘pending’, ‘partially paid’, ‘in process’, etc. It provides an overview of the bill’s progress and payment status.
Insurance File : This refers to any documents or files related to the patient’s insurance claim. It includes insurance policy details, claim forms, and correspondence with the insurance provider.
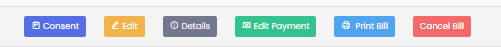
Consent
Consent typically refers to the patient’s or guardian’s agreement to the terms
of treatment and associated costs. This indicates that the patient has
provided their authorization for the treatment and acknowledges the costs
involved. It is an essential step before any billing or treatment can proceed.
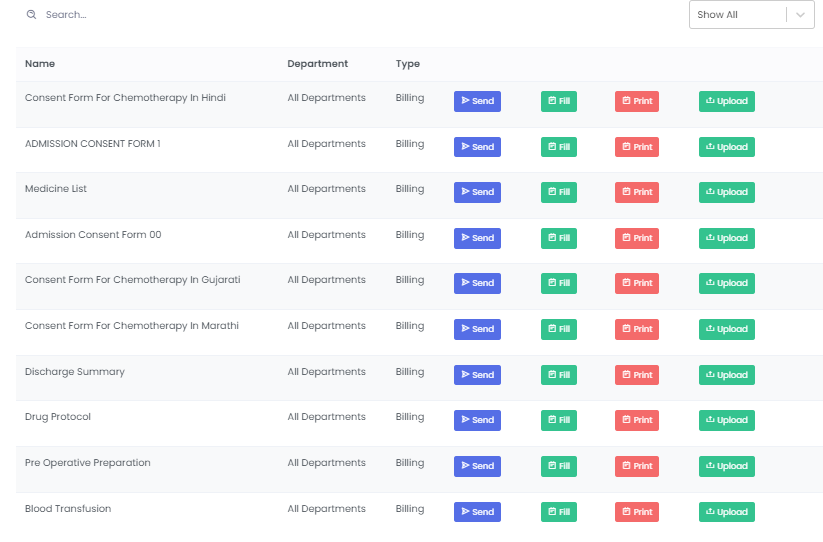
We can send the consent forms to patient or guardian to fill it
Edit
To make changes or modifications to existing information. This allows authorized personnel to modify or correct information on a bill. This could include changes to the patient’s personal information, the services provided, or the cost of those services.

Details
The specific information or data regarding a particular bill. This term refers to the comprehensive information about a patient’s bill, including itemized charges for treatments, medications, and other services rendered. It provides a full breakdown of all charges.

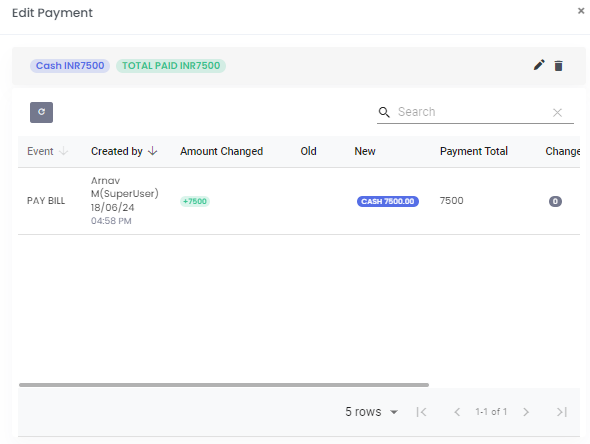
Edit Payment
The process of modifying the payment information. This allows hospital staff to update or correct payment details. This could involve changing the payment method, adjusting the amount paid, or correcting any errors in the payment records.
Print Bill
To produce a hard copy of the billing statement. This action generates a physical copy of the patient’s bill for records, patient review, or insurance claims. It includes all details of the charges and payments associated with the patient’s treatment.
Cancel Bill
To nullify or void a billing statement. This action is taken to invalidate a bill, which could be necessary for various reasons such as billing errors, duplicate entries, or changes in treatment plans. Cancelling a bill removes it from the active billing records and ensures it is not processed for payment.